“Women’s health needs to be front and center – it often isn’t, but it needs to be.”
– Cynthia Nixon
A common condition of the reproductive system known as pelvic inflammatory disease (PID) is commonly misdiagnosed and treated insufficiently. By screening asymptomatic patients for sexually transmitted infections (STIs) and rapidly treating those who have them in addition to PID, it is possible to prevent PID and its consequences, such as infertility, ectopic pregnancy, and persistent pelvic pain.
The Health Capital brings to you this blog to spread more awareness about pelvic inflammatory disease. It is unknown how many women experience PID each year, and it is likely underdiagnosed frequently. Between the ages of 15 and 24 is when it most frequently occurs in females.
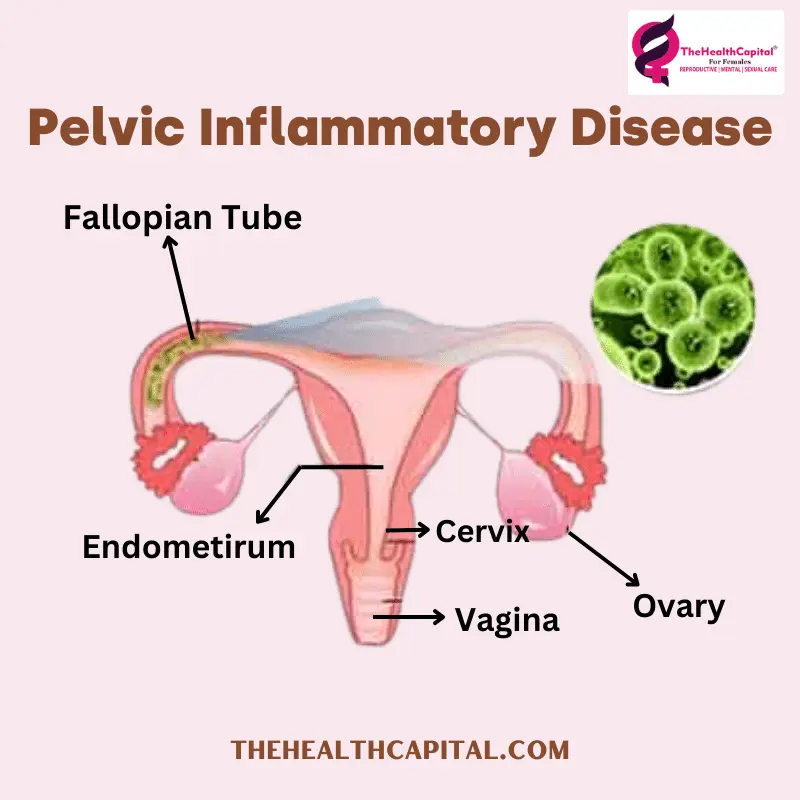
What is Pelvic Inflammatory Disease (PID)?
Pelvic inflammatory disease (PID) is an infection of a woman’s uterus, ovaries, or fallopian tubes. It might be caused by an infection that rises from lower genital organs, like the vagina or cervix. Untreated sexually transmitted infections are a common source of its acquisition (STIs). PID may also occur as a result of medical operations disturbing organisms that are naturally present in the lower genital tract.
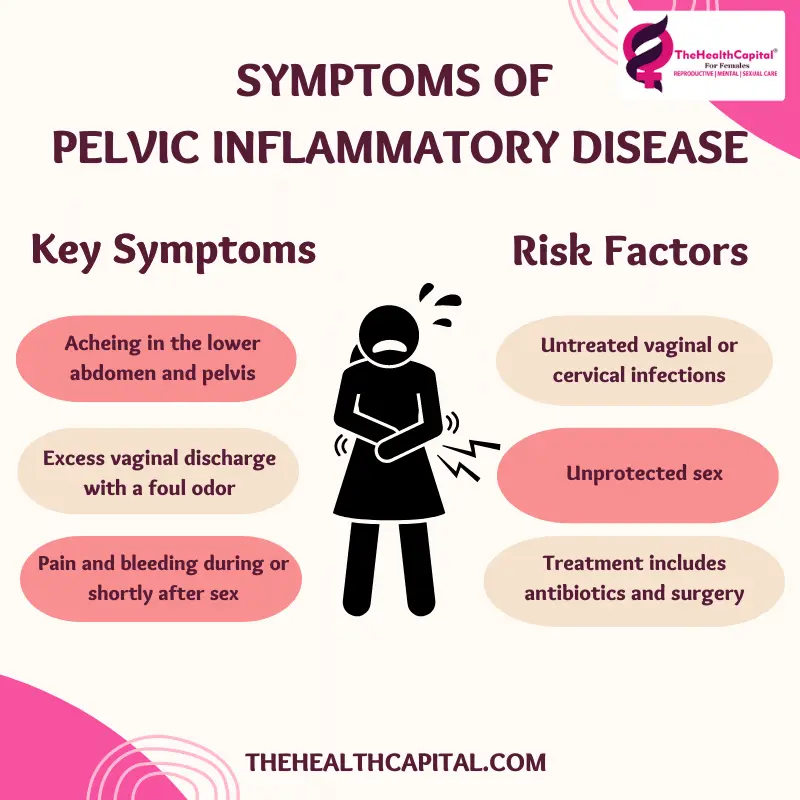
You are more likely to get PID if you have ever:
- A recent switch in sex partners. The danger increases as the number of partners increases.
- An earlier case of STI or PID.
- An abortion recently.
- A recent womb surgery or operation (uterus).
- A recently implanted intrauterine system or intrauterine contraceptive device (coil).
Pelvic Inflammatory Disease Symptoms
The signs and symptoms of pelvic inflammatory disease are as follows:
- One of the most typical Pelvic Inflammatory Disease Symptoms is pain in the pelvic area, which is located in the lower abdomen. Mild to severe variations are possible.
- Abnormal vaginal bleeding, which happens in roughly 1 in 4 cases, is another one of the signs and symptoms of pelvic inflammatory disease that could appear. This can include bleeding after intercourse, bleeding between periods, or periods that are heavier than usual.
- Suffering when having sex is also a symptom of pelvic inflammatory disease.
- Abnormal discharge from the cervix.
- A high degree (fever).
- A sore back.
Sometimes signs and symptoms of pelvic inflammatory disease come on gradually and mildly. For instance, you might just experience minor abdomen pain that ‘grumbles on for weeks. Sometimes you may not have any Pelvic Inflammatory Disease Symptoms and be unaware that you are infected. Even if you first show no symptoms of pelvic inflammatory disease, you are still in danger of consequences.
What tests may be done for Pelvic Inflammatory Disease?
- A little sample (swab) of discharge is typically collected from the neck of your womb if PID is suspected (cervix). This is a check for any bacteria (bacteria). Additionally, blood and urine tests, urethral swabs, and urine and blood tests may be performed. These are used to check for infectious microorganisms or infection-related signs and symptoms of pelvic inflammatory disease.
- The tests and swabs may occasionally fail to detect any germs. To support a PID diagnosis, more testing could be required. For instance, a blood test could reveal some infection or inflammation, and an ultrasound could reveal swollen Fallopian tubes. Sometimes there are further scans.
- Your womb (uterus) and tubes may need to be seen within your belly if your doctor has specific concerns. During general anaesthesia, a laparoscope—a narrow telescope—is introduced into your stomach wall. It’s known as a laparoscopy. The diagnosis of PID does not frequently need laparoscopy.
- If signs and symptoms of pelvic inflammatory disease are minor or do not appear at first, Pelvic Inflammatory Disease may not be diagnosed for some time.
- Also typically performed on women suspected of having Pelvic Inflammatory Disease is a pregnancy test. This is because an ectopic pregnancy and PID occasionally have identical symptoms. A pregnancy that develops in a Fallopian tube is known as an ectopic pregnancy and can lead to major issues.
Possible complications of Pelvic Inflammatory Disease
- If PID is identified and treated early, complications of pelvic inflammatory disease don’t usually arise. There could be one or more of the following issues:
- Another complication of pelvic inflammatory disease is having trouble getting pregnant (infertility). The Fallopian tubes may become damaged or scarred as a result of PID. Whether or whether the PID led to symptoms, this is still possible.
- If you get pregnant, you run a higher risk of the pregnancy growing in a Fallopian tube (an ectopic pregnancy). This is because the virus has harmed the Fallopian tube. There is a 1 in 10 probability that your pregnancy will be ectopic if you have had PID.
- The possible development of chronic pain is also a complication of pelvic inflammatory disease. This frequently includes sex-related suffering.
- Pregnant women with untreated PID are more likely to experience some pregnancy issues, such as miscarriage, early birth, and stillbirth.
- Inflammatory arthritis: It is rare for arthritis and ocular inflammation to be caused by this. It is a rather uncommon PID complication. In rare instances, it is hypothesized that the immune system ‘over-reacts’ to a pelvic infection.
If the infection is severe, an abscess (a collection of pus) may occasionally form adjacent to the uterus.
If you start treatment within 2-3 days after the onset of symptoms, you are less likely to experience problems. This can be feasible if symptoms appear suddenly. Some PID-afflicted women, however, experience just minor symptoms or none at all. The infection may progress for quite some time before it is diagnosed or treated.
Treatment for Pelvic Inflammatory Disease.
Treatment of PID aims to cover all potential bacteria and germs that could result in PID. PID can be treated with a variety of different regimens. It’s crucial to complete the entire course of pelvic inflammatory disease treatment.
If PID is detected, pelvic inflammatory disease treatment will often begin as soon as feasible. Sometimes, this may occur even before the availability of the results of samples (swabs) or another test. This is because the earlier therapy begins, the better the prognosis, and the lesser the chance of subsequent fertility issues.
If you believe you may be pregnant, let your doctor know. The choice of medicine may be impacted by this. An operation is occasionally required. For instance, if an abscess forms, drain it (which is very uncommon). Until both you and your sexual partner have finished pelvic inflammatory disease treatment, you shouldn’t have sex.
Does your partner need to be treated?
- Yes. Additionally, pelvic inflammatory disease treatment includes a test for the infection that should be performed on any other sexual partners from the previous six months. Your most recent sexual partner, regardless of how long ago the relationship was, should be tested and treated if you haven’t had sex in the last six months. Whether or not an infection is discovered after testing, prompt treatment is typically suggested. Because Chlamydia is a common cause of PID. It is frequently transmitted during sex.
- Although they frequently show no signs of having chlamydia, men can nonetheless transmit the virus.
- The chlamydia test’s accuracy is not perfect. The pelvic inflammatory disease treatment guarantees the eradication of any potential infection that the tests could have missed.
- Chlamydia may return to you after pelvic inflammatory disease treatment if your sexual partner is infected and not cured.
Can pelvic inflammatory disease be prevented?
When having sex, using a condom can help prevent STIs. With each change in a sexual partner, the risk of infection rises. View the Safer Sex booklet, which is distinct. If you are under 25 and sexually active, you should get tested for chlamydia once a year or if you switch partners. You can get a test done and You do not need to be examined to take the test. You will be requested to provide a sample of your urine, or in some cases, a sample (swab) from your lower vagina (a cotton wool bud is used to wipe the area).
Will it happen again?
- Every fifth woman with PID experiences another episode. Usually, this happens in two years. If your sexual partner was untreated, for example, this might happen. You risk contracting the virus once more after that.
- if the antibiotics were not taken correctly or long enough. The infection might not then entirely go away and might later return.
- If you switch partners and don’t engage in “safer sex” by using condoms.
- When a woman’s womb (uterus) or tubes have been harmed by a prior episode of PID, she may be more susceptible to infection.
The Health Capital Is Here For You
It takes a cycle to keep up a positive, healthy lifestyle. You can receive a free health analysis test from the convenience of your home through The Health Capital for which we have reproductive health consultants for females. We recognize that it might be challenging to get in touch with your consultants at times, but don’t worry—our goal is to raise awareness as widely as we can while also supporting our neighbourhood.
FAQ’s
1. What causes pelvic inflammatory disease?
An infection that starts to spread to the female reproductive system causes PID, also known as a pelvic inflammatory disease. A bacterial infection that enters the body through the cervix or vagina and then spreads to the womb, fallopian tubes, and ovaries is often what causes the sickness.
2. How serious is pelvic inflammatory disease?
Pelvic inflammatory disease (PID) is an infection of one or more of the upper reproductive organs, including the uterus, fallopian tubes, and ovaries (PID). PID that is left untreated can lead to the development of scar tissue and abscesses (pockets of infected fluid), both of which can permanently damage the reproductive system.
3. Does pelvic inflammatory disease show on ultrasound?
An ultrasound test may be performed on you. Scans can detect severe PID but cannot detect moderate illness. Even with a normal scan, PID is still conceivable.
4. Can amoxicillin treat pelvic inflammatory disease?
No serious negative side effects were reported with any treatment. The results of this comparative study suggest that oral Amoxycillin/clavulanic acid (augmentin) may be a useful alternative to the triple-drug regimen usually prescribed to treat pelvic inflammatory illness. As a result, the answer to the question “can amoxicillin treat pelvic inflammatory disease” is “yes.”
5. How to diagnose pelvic inflammatory disease?
The tests include-
a. A blood or urine test.
b. A pregnancy test.
c. A vaginal ultrasound scan, which is often performed with a probe (transvaginal ultrasound)

